The Center for Disease Control and Prevention (CDC) reports that the incidence of newly diagnosed type 2 diabetes mellitus has increased by 90 percent in the last 10 years.¹ However, it is more alarming that 46 percent of diabetic patients are unaware that they are affected and 42 percent are not confident in managing their diabetes.²  Rates for diabetes are rising for all groups, but especially among young people and race/ethnic groups. As primary eye care providers, it is imperative that we educate patients on the effects that diabetes can have on their vision, ocular, and systemic health. Education should include an explanation of the ophthalmic and systemic complications (including vision loss and possible low vision needs), frequency for eye and systemic examinations, prevention methods, and management. This is especially true for minority and lower socioeconomic populations. Pediatric cases also need to be considered.
Rates for diabetes are rising for all groups, but especially among young people and race/ethnic groups. As primary eye care providers, it is imperative that we educate patients on the effects that diabetes can have on their vision, ocular, and systemic health. Education should include an explanation of the ophthalmic and systemic complications (including vision loss and possible low vision needs), frequency for eye and systemic examinations, prevention methods, and management. This is especially true for minority and lower socioeconomic populations. Pediatric cases also need to be considered.
How does diabetes affect the eyes?
Diabetes is the leading cause of preventable blindness in the world. Particularly, it can increase risk for retinal damage, cataracts, and glaucoma. Damage is caused by compromised  vasculature leading to bleeding and fluid accumulation in the macula causing vision loss. Eric Dollar, O.D., from Austin, Texas, describes retinal images to his patients as “the only place you can look at blood vessels without cutting your skin, and these are the same blood vessels throughout the rest of your body including your heart, brain, kidneys, feet etc”. Explaining that diabetic changes in the eye are a representation of complications that can happen all over the body can help to stress the gravity of this condition during the education portion of the comprehensive eye exam.
vasculature leading to bleeding and fluid accumulation in the macula causing vision loss. Eric Dollar, O.D., from Austin, Texas, describes retinal images to his patients as “the only place you can look at blood vessels without cutting your skin, and these are the same blood vessels throughout the rest of your body including your heart, brain, kidneys, feet etc”. Explaining that diabetic changes in the eye are a representation of complications that can happen all over the body can help to stress the gravity of this condition during the education portion of the comprehensive eye exam.
When should you check for diabetes?
The Diabetes Control and Complications Trial presents retinopathy as one of the earliest complications of diabetes, being able to be detected as early as 6.5 percent of HbA1c for intensive glycemic control. Therefore, annual eye examinations play a major role in diagnosis. The American Diabetes Association (ADA) recommends that all patients should be screened for diabetes starting at age 45.³ However, patients who are overweight and have conditions such as hypertension, hypercholesterolemia, cardiovascular disease, dyslipidemia, polycystic ovary syndrome, or family history of diabetes are recommended for diabetes screening at any age.³ Patients with Type 2 diabetes should have an eye examination at the time of diagnosis. It can be effective to mention that diabetes affects the vasculature when educating patients on retinal findings. 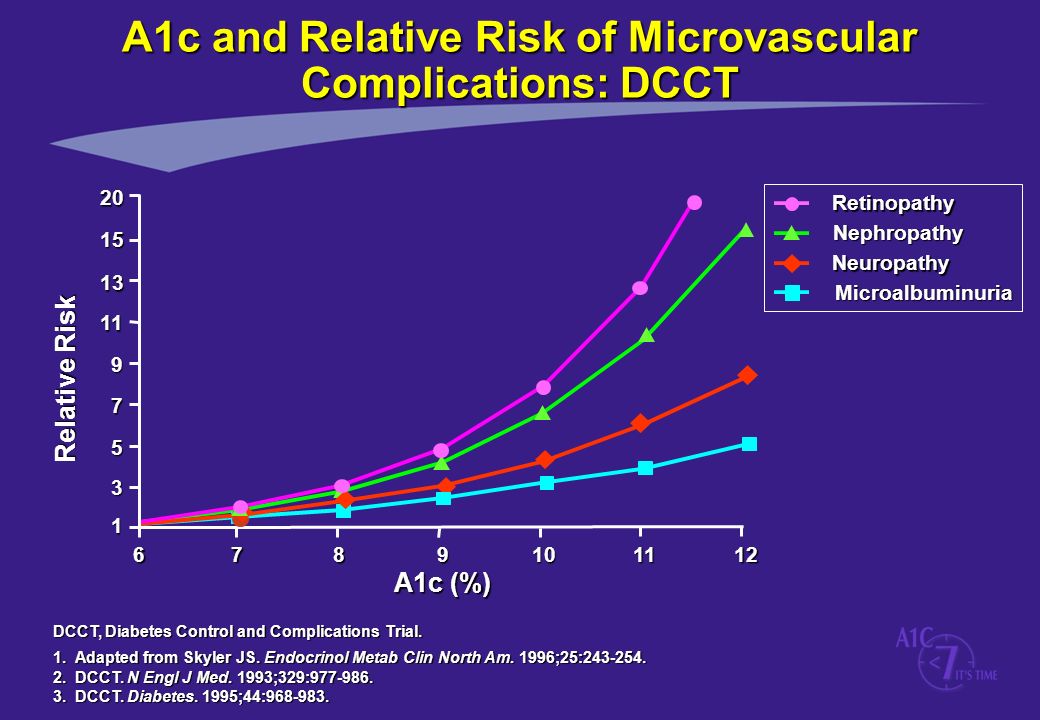
How can you prevent diabetes?
Apart from regular visits with healthcare providers, diet and physical activity can help prevent the risk of developing diabetes. Patients should be educated on maintaining a healthy diet including increasing the intake of fiber and whole grains which can regulate blood sugar levels. Additionally, the ADA recommends 30 minutes of physical activity three times a week. As a rule of thumb, for every kilogram (or 2.2 pounds) of weight lost, there is a 16 percent decrease in diabetic progression risk.⁴ Good weight control is the No. 1 preventable risk factor on which we can advise patients.
Besides diet and exercise, medication is also key. Systemic oral and injectable medications can assist in blood sugar control of Type 1 and 2 diabetes. If an individual with ocular complications from diabetes advances to proliferative retinal disease, vascular endothelial growth factor inhibitors (anti-VEGF injectable medications) are widely prescribed as a first line therapy to prevent the progression of more advanced disease. In fact, these anti-VEGF injectable medications have been shown to improve visual acuity in cases of diabetic macular edema. With or without VEGF injections, patients with diabetes should plan for annual comprehensive dilated eye examinations and more frequent retinal follow-ups by an eye care provider. Eye health examinations go a long way toward managing diabetes.
How can you manage diabetes?
Simplifying management can increase patient understanding and compliance with treatment. Patients should be introduced to the simple ABCs of diabetes management, which are modifiable risk factors including⁶:
A = Hemoglobin A1c. In general, 1 percent decrease in HbA1c level leads to a 40 percent decrease in risk for microvascular complications. Intensive glycemic control is critical in ALL individuals with Type 1 and Type 2 diabetes.
 B = Blood pressure. In general, each decrease of 10 mmHg in systolic blood pressure decreases the risk of diabetic complications by 12 percent. High blood pressure (hypertension) has been shown to make diabetic retinopathy and systemic complications from diabetes progress faster.
B = Blood pressure. In general, each decrease of 10 mmHg in systolic blood pressure decreases the risk of diabetic complications by 12 percent. High blood pressure (hypertension) has been shown to make diabetic retinopathy and systemic complications from diabetes progress faster.
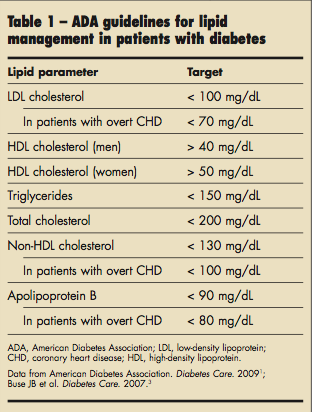
C = Cholesterol and dyslipidemia. Accurate management of lipid levels is important for controlling diabetic complications and progression. A general guideline of cholesterol/lipid levels is listed in this table.⁵ Dyslipidemia has been shown to make diabetic retinopathy and systemic complications from diabetes progress faster.
s = Smoking. Smoking leads to a statistically significant increase in the risk of diabetes and diabetic complications. The risk is greater for heavy smokers, and can last even after cessation of smoking.⁷
In addition to patient education, it is good practice to co-manage findings with other healthcare providers participating in the patient’s care. Clearly communicating exam findings and recommendations to involved providers further facilitates holistic care for our patients. As diabetes rates increase, the profession of optometry should proactively address the condition and do our part in its prevention, diagnosis, and management. The AOA’s Evidence-Based Clinical Practice Guideline: Eye Care of the Patient with Diabetes Mellitus provides important guidance on the topic.
About John  Raji
Raji
John is an optometry student in his fourth year at the University of Houston College of Optometry. John is heavily invested in OptometryStudents.com with various roles including: Director of Team Development, Executive Editor, and Executive Journalist. He is the Sports Vision Section liaison for the American Optometric Association and has a strong interest in Cornea and Contact Lenses. John enjoys graphic design, music and exploring the outdoors.
References:
- Klonoff, David C. The Increasing Incidence of Diabetes in the 21st Century. Journal of diabetes science and technology (Online). 2009;3(1).
- Centers for Disease Control and Prevention. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services 2014.
- American Diabetes Association. Standards of medical care in diabetes—2015 abridged for primary care providers. Clinical diabetes: a publication of the American Diabetes Association. 2015;33(2):97.
- Hamman, Richard F. et al. Effect of Weight Loss With Lifestyle Intervention on Risk of Diabetes. Diabetes Care. 2006;29(9):2102–2107. PMC. Web. 11 Sept. 2017.
- American Diabetes Association. American Diabetes Association clinical practice recommendations 2001. Diabetes Care. 2001;24(1):1-133.
- Abbate, Samuel L. Expanded ABCs of diabetes. Clinical Diabetes. 2003;21(3):128-133.
- Willi, Carole, et al. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298(22):2654-2664.


