Background
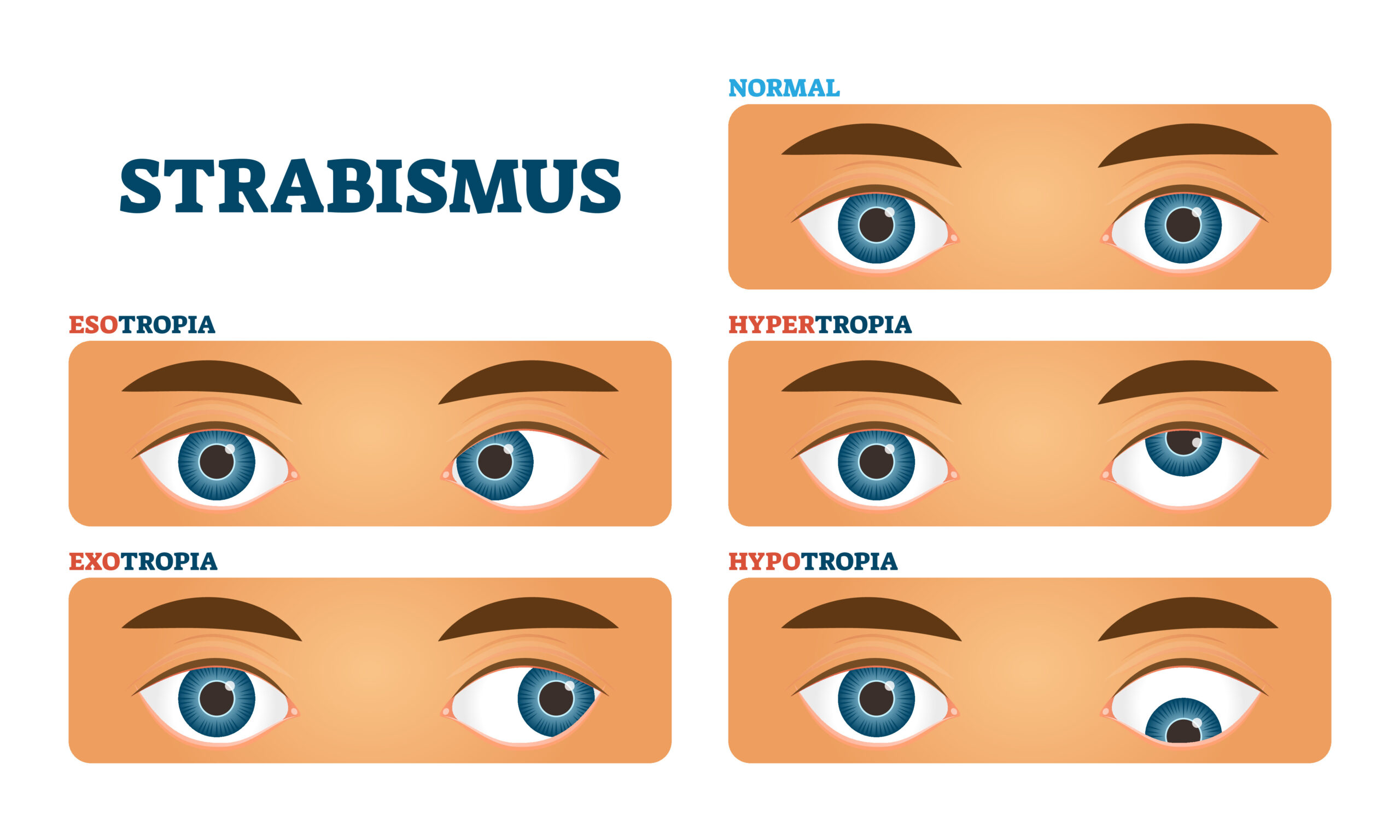
A Cover Test is one of the skills learned during the first year of optometric education, and it is an important part of a comprehensive eye examination. This test is used to evaluate and quantify ocular deviations that may be present, which are called tropias and phorias. A tropia is a physical misalignment in one or both eyes that can also be called strabismus.1 On the other hand, a phoria is a deviation that may only be present when the eyes are not looking at the same object. One key difference: whether fusion is maintained or not.
Approximately 4% of the US population has strabismus, which is about 13 million people, all of whom likely went to their eye doctor and had a cover test performed.2 The range of deviations is wide, from a small microtropia (less than 10 prism diopters) to a large angle tropia that can deprive the patient of stereopsis or may result in amblyopia. To make sure that you are solid on the basics, here is a cover test breakdown to help assess eye deviations like a pro.
What you need:
- Near target (for near cover test)
- Visual acuity chart (for distance cover test)
- Occluder
- Vertical and horizontal prism bars
- Overhead lamp
- Patient’s habitual correction
Parts of the cover test
To test for the different types of deviations and quantifying their magnitude, the cover test is divided into two main parts: the “unilateral” or “cover-uncover” test and the “alternating” cover test. Both parts of the evaluation are performed at distance and at near.
The cover-uncover test is done first to determine if a patient has either a phoria or a tropia. The alternating cover test, on the other hand, is used to measure the magnitude and direction of a deviation, regardless of whether it is a phoria or a tropia.3
Unilateral Cover Test (UCT)
Purpose and Setup. The unilateral cover test is performed first and, like the name suggests, is focused on what one eye does when fusion is broken. It is to be performed while the patient wears any applicable habitual correction. For example, if the patient only wears glasses for distance, perform distance testing with the glasses on, then remove the glasses for near testing. Instruct the patient to look at the target and keep it clear. The target for both distance and near testing should be a single letter, one or two lines above the patient’s best corrected visual acuity. The near target should be held approximately 40 cm away from the patient.4
Performing UCT. For this test, one eye is covered with the occluder. During this time, the you should look at the opposite (unoccluded) eye to see if it moves to pick up fixation. For example, if you start by covering the right eye, you should immediately look at the left eye to see if there is movement. This process of covering and uncovering the same eye is repeated 2-3 times to verify your observation before moving over to perform the test in the fellow eye.
Results. If no movement was observed in the eye that remained uncovered while performing the test, then the patient has a phoria. This means that both eyes were aligned with the target.4 If there was a movement while testing either of the eyes, then the patient has a tropia. This indicates that both eyes are not fixating on the target simultaneously.
Alternating Cover Test (ACT)
Purpose and Setup. When performing an alternating cover test, you will use the same targets and testing distances as with unilateral cover test.
Performing ACT. This part of the test also starts with instructing the patient to keep the target clear, but now the goal is to get the magnitude and direction of the deviation. To do this, place the occluder over one eye for 2-3 seconds, and then move it to the opposite eye. While alternating the occluder from eye to eye, you should be looking at the eye that was just uncovered to see in what direction it moved. For example, imagine that you covered the right eye for 2-3 seconds, then you cover the left eye while looking at the right eye to see if it moved when you uncovered it. You repeat this movement several times. If the uncovered eye swings out, that means the eye was turned in to begin with and had to rotate in an outward motion to obtain fixation. The same holds true for opposite; when the uncovered eye swings in, that means it was turned out to begin with.
Results. After the direction of the deviation has been identified, it is time to measure the magnitude with the help of the prism bars. To do this, a prism can be placed in front of one of the eyes as you repeat the alternating cover test. If the patient has a tropia, place the prism in front of the deviating eye. For phorias, the prism could be placed in front of either eye. The direction of the base (the thickest part of the prism) depends on the direction of the deviation. As the examiner repeats the alternating test with the prism in front of one of the eyes, the amount of prism power is increased until no movement is seen in that eye.3 This means that the misalignment has been neutralized with that prism.
Neutralizing with ACT
The direction of the deviation seen in the alternating cover test is what dictates the placement of the prism base to measure the magnitude of the misalignment for neutralization. When the eye moves in as it is being uncovered, it is considered to have an exo deviation, which can be an exophoria or exotropia. In other words, the eye was originally turned out and had to move inward towards midline to pick up fixation. When the eye moves out as it is uncovered, the deviation is termed eso and could be classified as an esophoria or esotropia. In other words, the eye was originally turned in and had to move outward towards midline to pick up fixation.
It is important to note that even if no motion is seen on cover test, prism bars should still be used to “bracket” the horizontal phoria. To perform a bracket, hold up 2-4 prism diopters of base in prism and look for a reversal, which means the patient is unable to handle the deviation and you will see motion in the opposite direction. For example, if you hold up a small amount of base out prism over the left eye of an orthophoric patient, you should expect to see the right eye swing out due to Hering’s Law of Equal Innervation. The base should then be switched to the opposite orientation and the alternating cover test should be performed again. If the patient is truly orthophoric, you would expect the 2-4 prism diopters to cause motion of equal magnitude with both directions of the base. It is also a good idea to perform this on all patients you note as “ortho” because it is a skill you are expected to perform on the National Boards!
In addition to the horizontal deviations of exo and eso, the eyes can also deviate vertically. When the eye moves down to pick up fixation as it’s being uncovered, it is termed a hyper deviation, either hypertropia or hyperphoria. When the eye moves up in order to fixate, it is a hypo deviation, either hypotropia or hyperphoria.
Base Direction
To neutralize the different types of deviations, place the base of the prism in the following orientation:
- Hypo deviations: base up
- Hyper deviations: base down
- Eso deviations: base out
- Exo deviations: base in

Practice, practice, practice!
Becoming comfortable with performing a cover test can take time, so practice on as many classmates and family members as possible. Remember: always start with the unilateral cover test to identify if a tropia or phoria is present and continue with the alternating cover test to observe both the direction and magnitude with the use of prisms.
Even though the cover test has several parts and many rules to accurately classify ocular deviations, it gets easier with practice, and most of the test indications become second nature after performing it several times.
References
- Leitman, M. W. (2017). Manual for Eye Examinations and Diagnosis. Ninth ed.. Hoboken, New Jersey; John Wiley & Sons. 2017.
- American Academy of Ophthalmology. 2019. Cover Tests. [online] Available at: <https://www.aao.org/bcscsnippetdetail.aspx?id=5051fd44-4106-4b1a-bf19-00566baa0b07> [Accessed 24 August 2020].
- American Academy of Ophthalmology. 2019. Cover Tests. [online] Available at: <https://www.aao.org/bcscsnippetdetail.aspx?id=5051fd44-4106-4b1a-bf19-00566baa0b07> [Accessed 24 August 2020].
- Carlson, B. Nancy, Kurtz, Daniel. Clinical Procedures for Ocular Examination. 3rd New York; McGraw-Hill. 2004.

