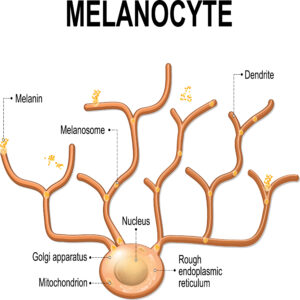
 Background: A choroidal melanoma is a malignant tumor of choroidal melanocytes. The melanin-containing cells in the choroid become malignant and grow underneath the RPE. This type of tumor is the most common primary intraocular malignancy in adults; additionally, it is more prevalent in Caucasian patients and is usually found around fifty to sixty years of age. (2)
Background: A choroidal melanoma is a malignant tumor of choroidal melanocytes. The melanin-containing cells in the choroid become malignant and grow underneath the RPE. This type of tumor is the most common primary intraocular malignancy in adults; additionally, it is more prevalent in Caucasian patients and is usually found around fifty to sixty years of age. (2)
Symptoms: Patients are often asymptomatic, but they can have blurring or distortion of vision. Flashes of light (photopsias) and floaters (myodesopsias) may be perceived by the patient. Decreased vision, visual field defects, and pain may also occur. (1)

Signs: Choroidal melanoma is usually seen as a pigmented, brown-grey, dome-shaped, subretinal elevation during a fundus exam. However, it can present as amelanotic (due to both the loss of pigment and an appearance of a yellow color) or appear relatively flat. Subretinal fluid, thickness of > 2 mm with an abrupt elevation of the choroid, congested blood vessels at the tumor apex, or a break in Bruch’s membrane with a subretinal hemorrhage are all also characteristic of choroidal melanoma. Growth is also common, especially if it occurs over a short period of time. Clumps of ill-defined, orange pigment (lipofuscin) are frequently seen on the surface of the lesion. Lipofuscin signals that the given area of the retina is metabolically active. Note that a diffuse melanoma can be minimally thickened without a prominent elevated mass, of which will appear similar to a nevus. (1)
Diagnosis: Case history should be carefully taken, asking questions concerning cancers, anorexia, weight loss, and recent illness. A melanoma is usually diagnosable based upon a dilated fundus examination. B-scans will show low-to-moderate reflectivity with choroidal excavation and thickness of often > 2 mm. A mushroom appearance is characteristic and can be observed on B-scan where the melanoma has broken through Bruch’s membrane into the vitreous. An OCT can document thickness as well as subretinal fluid. ICGA will display double circulation, with prominent blood vessels within the melanoma. A fine-needle aspiration biopsy can be done, usually for prognosis and genetic analysis versus diagnostic purposes. (1)
Referral: If a choroidal metastasis is anticipated or suspected, referral to an internist or oncologist should be made for a breast examination, full skin examination, chest CT, bloodwork, and other relevant testing. This extensive workup determines metastatic status.
 Treatment: Treatment is determined by several factors, including but not limited to: age of the patient, general patient health, metastatic status, tumor characteristics, and status of the non-cancerous eye. Procedures for treatment can include: observation, photocoagulation, transpupillary thermotherapy, irradiation (most commonly brachytherapy), local resection, enucleation, and exenteration. (2)
Treatment: Treatment is determined by several factors, including but not limited to: age of the patient, general patient health, metastatic status, tumor characteristics, and status of the non-cancerous eye. Procedures for treatment can include: observation, photocoagulation, transpupillary thermotherapy, irradiation (most commonly brachytherapy), local resection, enucleation, and exenteration. (2)
Prognosis: The earlier the diagnosis and treatment, the better the outcome. This condition has a better outcome if detected and treated before it has metastasized to other areas of the body. Metastasis from the eye to other organs often results in death of the patient. Once the choroidal melanoma has metastasized to the liver, the prognosis is not optimal, whether the melanoma has been treated or not. (2)
References:
- Bagheri, N., & Wajda, B. (2017).The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease (Seventh ed.). Philadelphia: Wolters Kluwer.
- Bowling, B., & Kanski, J. J. (2016). Kanski’s Clinical Ophthalmology : a Systematic Approach (8th ed.). Edinburgh: Elsevier.

