Tracy Voegeli of SUNY 2013 is the winner of the December 2012 Clinical Case Review. This is the premier resource for optometry students to post their most interesting optometric clinical cases online for all to see. A winner will be chosen monthly and will receive a clinical gift bundle, an official certificate signed by the founder of OptometryStudents.com and their clinical case will be promoted for the optometry community to see and enjoy.
Age / Sex / Race
61 Year Old White Female
Chief Complaint
Complaining of distance and near vision blur that became bothersome a few months ago. The patient was wearing single vision distance specs and single vision near specs that were about 4 years old, the lenses were very scratched.
Medical History
(+) History of stoke 4 years ago with left sided weakness. Patient was vague about details but reports a full recovery
(+) HTN. Controlled with Amlodipine
(+) Depression. Controlled with Seroquel, Prozac
(+) Hyperlipidemia. Controlled with Crestor
Ocular History
— LEE 1 year ago
— BCVA 20/30 OD/OS. Reduced VA attributed to nuclear cataracts.
— Bifocals prescribed. The patient reports they do not wear the new bifocals because could not adjust to new lens form.
(-) Flashes, Floaters, diplopia, BIRT
Other History (Allergies, Family History, Refractive Error) Refractive error: Compound hyperopia astigmatism, Presbyopia
(+) Allergy to dust
(-) Family History
What did you think the diagnosis was and what was your initial plan of action?
At this point in the exam I am thinking the blur is related to a refractive issue or a result of the pt wearing older specs that are in poor condition. Also the patient had cataracts noted in the previous exam, and this could contribute to the chief complaint of blurred vision.
List any applicable testing and results of testing:
OD: 20/60-
OS: 20/25-2
Near acuity (habitual Rx)
OD: 20/70
OS: 20/50
Extraocular muscles: Full range of motion OD/OS
Pupils: PERRL –APD
Refraction:
OD: +3.75-0.25×80
BCVA: 20/60- // Pin hole No improvement
OS: +3.75-0.50×80
BCVA 25
Biomicroscopy:
Lids/lashes: Thickened lid margin, debris on lashes OD/OS
Conjunctiva: Clear OD/OS
Cornea: Clear OD/OS
Anterior Chamber: Deep and Quiet OD/OS
Angles: Open OD/OS
IOPs
OD: 15 mmHg
OS: 16 mmHg
Dilated Fundus Exam:
Lens: Grade 1 NS OD/OS
C/D: 0.20 OD/OS
Optic Nerve: Round, pink, obeys ISNT rule
Macula: OD Red Macula. (+) Watzke allen test
OS Flat, intact
Vascularture; Mild arteriole attenuation OD/OS
Periphery: Flat and intact no holes or tears 360 OD/OS
Vitreous: Synuresis OD/OS. No PVD noted OD/OS
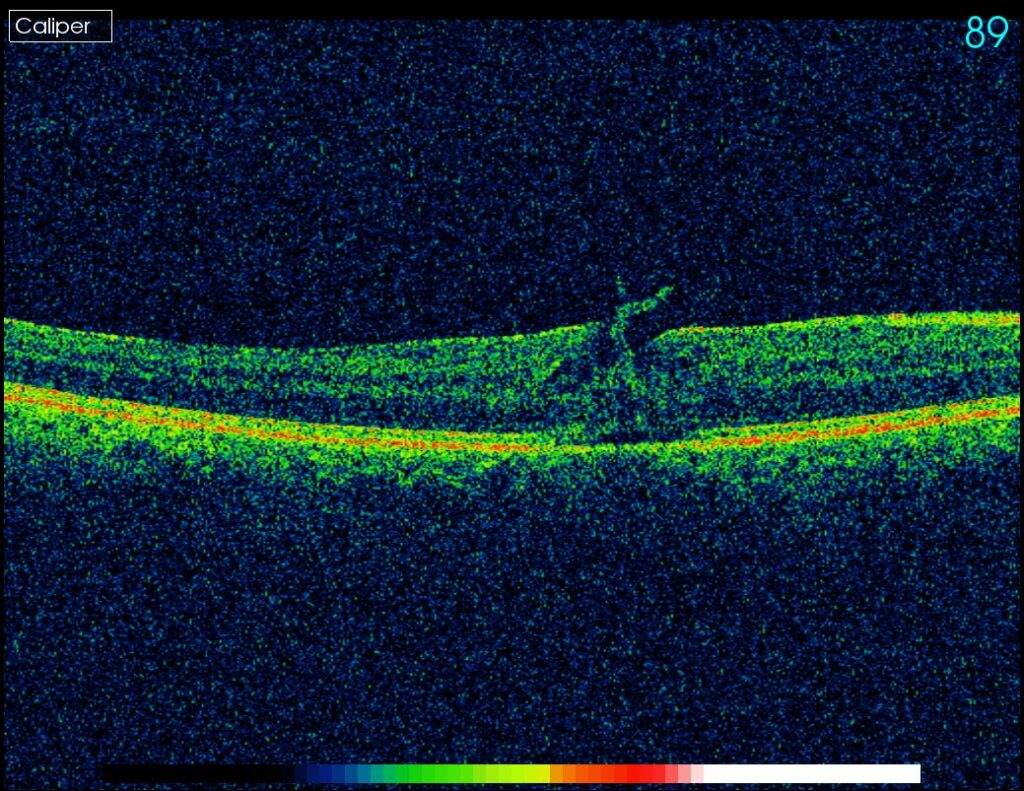
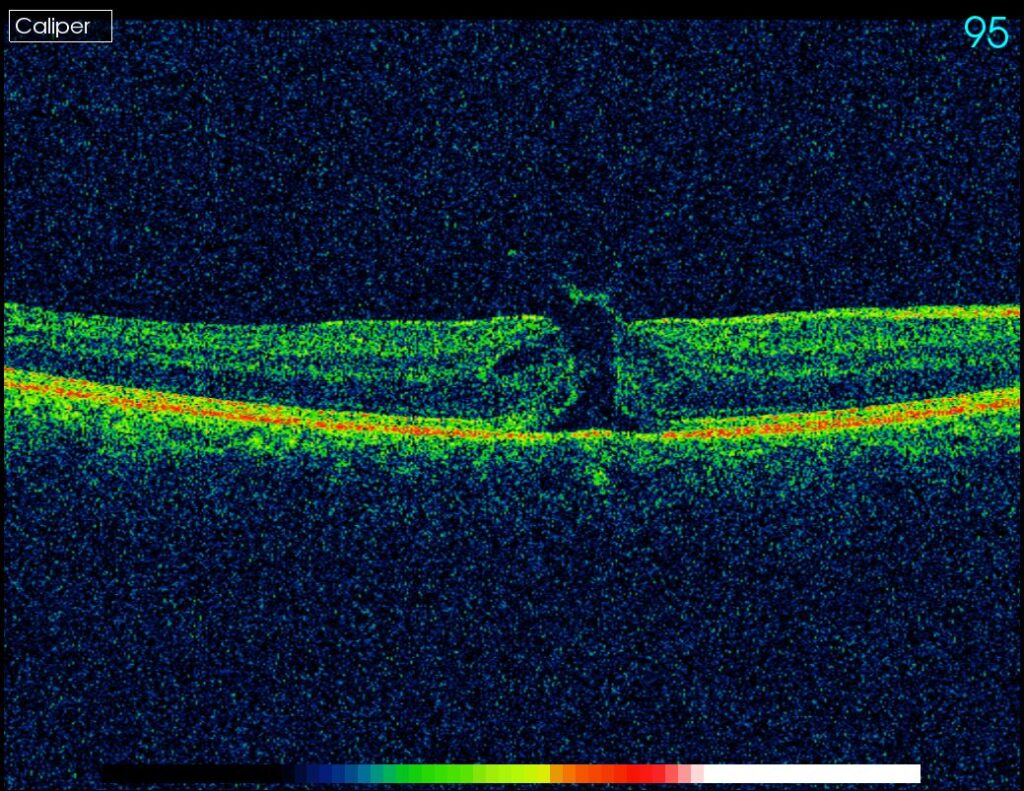
OCT:
OD: Macular hole with vitreal macular traction.
(-) cuff of subretinal fluid
Vitreal traction just inferior to fovea. OCT image 89
Macular hole inferior to fovea. OCT image 95.
List any differential diagnosis after your testing was complete and why:
After determining the refraction was not improving this patients VA, we needed to find the cause of the reduction in vision OD. One year ago the BCVA OD was 20/30. The patient’s only complaint was blurred vision. We began to move anterior to posterior to look for a cause of reduced VA. The anterior segment was normal, the lens had mild nuclear cataracts but not enough to account for this reduction in VA. Pupils were reactive, there was no APD so that rule out optic nerve problems or extensive retinal damage. The patient had a history of hypertension and stroke so I was thinking something vascular may have occurred such as a branch vein occlusion affecting the macula.
Once I dilated my patient I was able to rule out BRVO. For the most part the fundus of the right eye looked normal, except for the fact that the foveal area was redder then usual, and redder on comparison to the left eye. At this point I was suspecting a macular hole. This suspicion was confirmed with the Watzke Allen test and OCT.
In the presence of a full thickness hole the macula will appear red and can have a gray halo of subretinal fluid. A partial thickness holes is not a red as a full thickness hole and the grey halo is not usually seen. A pseudohole can be differentiated from a macular hole by the Watzke Allen test.
What was your assessment and plan? (include diagnosis, treatment and follow up):
Macular Holes are categorized into different stages.
Stage 1: impending hole
Stage 2: small full-thickness hole
Stage 3: Full thickness hole with cuff of subretinal fluid. (-) PVD
Stage 4: Full thickness hole with cuff of subretinal fluid. (+) PVD
The treatment of a retinal hole depends on the stage of the hole and the patients VA. Approximately 50% of Stage 1 holes will resolve spontaneously.
The treatment for a macular hole is a vitrectomy, membrane peel and gas injection. Following the surgery the patient is required to remain in a prone position with the head down for 7-14 days to allow the gas bubble to press against the macula.
The earlier a hole is treated the better the visual outcome. Holes in stage 2-4 with a VA of 20/40 can be treated. The prognosis is good for recent onset hole, but poor for holes that are greater then 1 year old.
Our patient had a small macular hole that was just inferior to the fovea with vitreal traction. We decided to refer our patient for a retinal consult.
Anything else you would like to add? (Lessons you learned, the patients response, advice to students etc.) This case was of particular interest to me because the complaint of blurred vision is a common complaint heard in a general practice setting and is commonly a result of refractive error.
This case was a reminder that a complaints of recent blurred vision can also mean ocular pathology.