Background: Fuchs’ Endothelial Dystrophy is an autosomal dominant, inherited, posterior dystrophy of the cornea. Fuchs’ is more common in post-menopausal females, with a predilection for women 60 years of age or older. Around 30% of patients have a family history of the condition.2
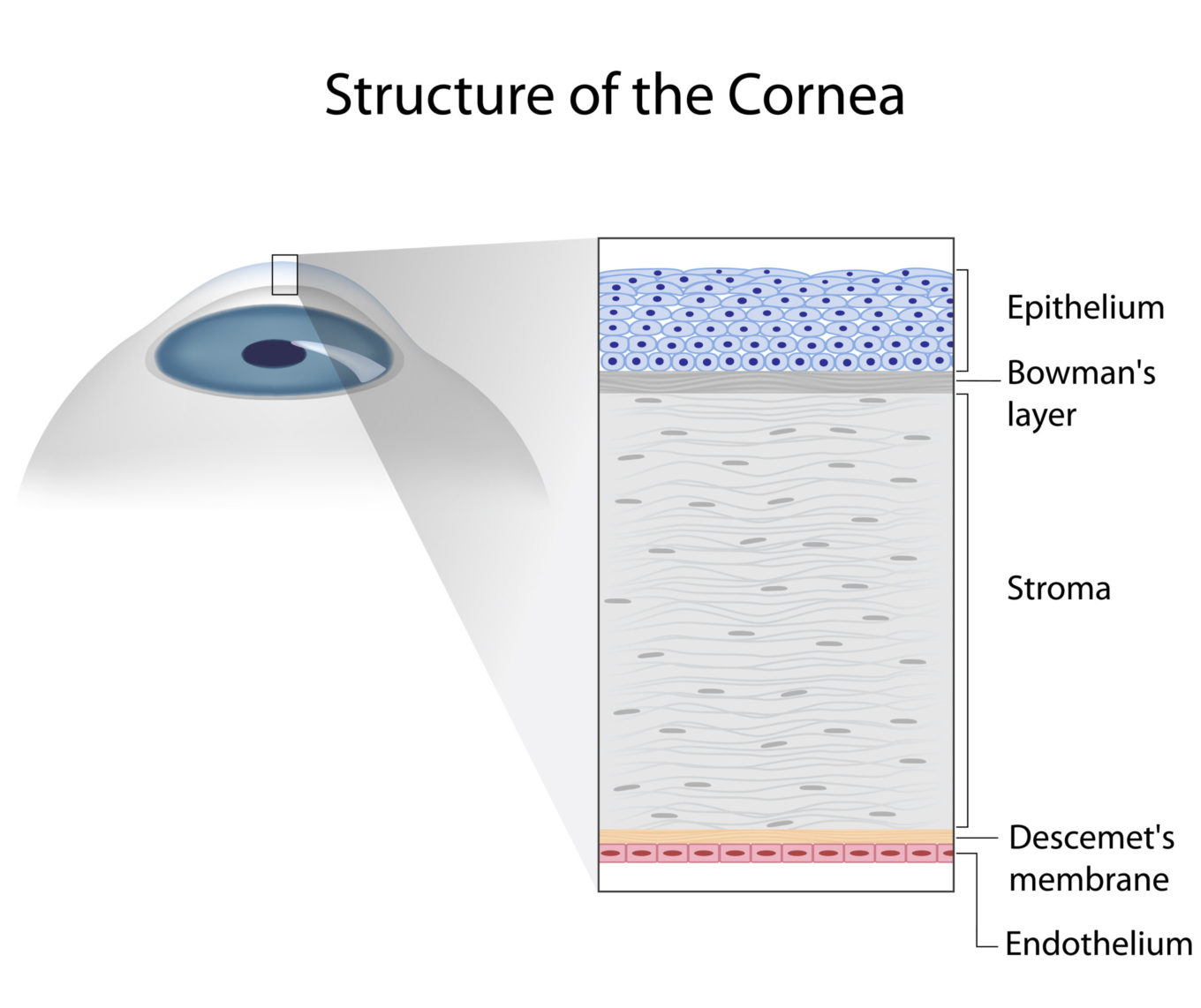
Pathophysiology: In Fuchs’ dystrophy, the posterior lamina of the Descemet’s membrane is produced in excess. This can be seen as clumps, gutatta, of basement membrane on Descemet’s membrane and are associated with a decrease in endothelial cell count density. The corneal endothelium is roughly five microns thick, and its number one function is to pump and produce Descemet’s membrane (type four collagen). When there is an excess of Descemet’s, endothelial cells are knocked out. Therefore, Descemet’s thickens and endothelium thins.
Decreased endothelial cell density is a hallmark of Fuchs’.2
Symptoms: Fuchs’ can occur in early age (30-40 years old); however, these patients are often asymptomatic until later on in life (50-60 years old). Progression of the disease can result in hazy vision in the mornings with accompanied pain and glare. The pain results from bullae.2

Signs: Endothelial cells undergo pleomorphism and polymegathism (change in cell shape and size, respectively), and endothelial guttata have a “beaten bronze” or “beaten metal” appearance. You will have thick pachymetry findings as this disease progresses. Loss of these corneal endothelial cells that have Na+/K+ pumps leads to inappropriate corneal thickness. Stroma edema will develop when the endothelial cell pumps are no longer able to maintain proper osmotic balance. This imbalance often occurs when cell count is less than 500 cell/mm2. As the dystrophy continues to progress and worsen, stroma edema will spill over into the epithelium, causing painful bullae within the epithelial layer, as well as scarring. (2)
Treatment: Sodium Chloride (Muro 128) is a hypertonic solution that is prescribed for the reduction of corneal edema. This hyperosmotic is available as an eye drop at 2% and 5% as well as an ointment at 5%. Additionally, serial pachymetry can be done to monitor thickness of the cornea and progression of the disease.2
When to Refer: A comprehensive exam is recommended every year, starting at 40-50 years old. As the disease progresses, guttata gradually become confluent and take on an “orange peel” look. They then get a central “plaque”, which is guttata on guttata with a very thick Descemet’s membrane. Subepithelial haze slowly develops amidst the chronic corneal edema, in which bullae and prominent fibrosis can occur at any time but typically occur after confluent guttata. Confluent guttata qualifies for an elective DMEK (Descemet Membrane Endothelial Keratoplasty); follow up would be every six months (or sooner if symptoms worsen) if surgery was differed. AM blur is a sign that surgery needs to be conducted soon. Bullae signal that surgery is urgent and needs to occur as soon as possible. Fibrosis is the point where surgery would be difficult, so referral needs to occur before the fibrosis stage.1
Surgery: Surgical treatment for advanced Fuchs’ would need to include a corneal transplant that replaces the endothelium, seeing as the cell loss occurs in the endothelial layer with this dystrophy. DSAEK or DMEK are options for the corneal transplant, as they replace the endothelium without being a full thickness transplant. Rejection rate as well as recovery time is longest for a full thickness corneal transplant, such as PK. For this reason, a surgeon will elect to not do a full thickness transplant. DSEAK and DMEK have the same implications, but DMEK is a little more difficult with ACIOL, pars plana vitrectomy, tubes, or large iris defects. However, the DSEAK donor contains stroma, of which the DMEK donor does not. DMEK is the surgery of choice where it has the shortest recovery time, at 1-2 weeks, and well as the lowest rejection rate, at 1%. Additionally, the Descemet’s’ membrane barrier stays intact with DMEK, so there is less edema with this transplant (unless there is an area where the donor isn’t attached yet).1
Cataract Surgery Implications: Cataract surgery will make a Fuchs’ patient worse, as the surgery will often knock the endothelial cells during the procedure. This increase in endothelial cell loss can accelerate the dystrophy, especially if the cell count is less than 1,000 cell/mm2. The normal endothelial cell count ranges from 3,000-4,000 cell/mm2 in children to 1,000-2,000 cell/mm2 in an eighty-year-old individual. A minimum of approximately 500 cell/mm2 is required in order to prevent edema. Often when a patient has advanced Fuchs’ as well as advanced cataracts, the surgeon will opt to do the cataract surgery followed by a corneal transplant.1
References:
- Bowling, B., & Kanski, J. J. (2016). Kanski’s clinical ophthalmology: a systematic approach (8th ed.). Edinburgh: Elsevier.
- Cheatham, K. M., Cheatham, M. A., Wood, K. B., & Kmk Educational Services, Llc. (2007). KMK part one : basic science review guide (12th ed.). Overland Park, Ks: Kmk Educational Services, Llc.

