June is Cataract Awareness Month. On behalf of OptometryStudents.com, I’m here to provide you with a crash course on the common types of cataracts, clinical signs to expect, and different types of cataract treatment (see Part 2). Cataracts are defined by the American Optometric Association as a “cloudy or opaque area in the normally clear lens of the eye,” and while they don’t often mature to be too debilitating here in the United States due to general widespread accessibility of surgical procedures, they are responsible for 51% of blindness worldwide. Patients’ most common complaint associated with cataracts is blurry vision, often associated with glare, so listen closely for complaints of “trouble watching TV” or “trouble driving at night!” Listed below are common forms of cataracts and characteristics about each.
Types of Cataracts
Nuclear Sclerotic Cataract
- Characterized by opacification of the center of the lens (i.e. the nucleus, hence “nuclear sclerotic”).
- Associated with increasing age.
- Often associated with a yellowing of the lens called “brunescence.”
- Decreases contrast and increases glare (patients often state they have trouble with “night driving”).
- May cause a myopic shift in refraction (as in, become more nearsighted). This is fairly unique because it can cause patients to have what is commonly referred to as “second sight.” This means a hyperopic (far sighted) patient may actually experience an increase in visual acuity with the onset of nuclear sclerotic cataracts, despite having decreased contrast and increased glare.
Cortical Cataract
- Characterized by spoke-like opacities traveling radially from the edge of the lens toward the center (the closer the spokes are to the visual axis, the more likely they are to affect vision).
- Associated with increasing age.
- Decreases contrast and increases glare (patients often state they have trouble with “night driving”).
- May cause a hyperopic shift in refraction (as in, become more farsighted). This effect is the opposite of the myopic shift caused by nuclear sclerotic cataracts.
- More likely to be seen in patients with diabetes mellitus. However, because an increase in blood sugar can cause a myopic shift, it’s not uncommon for diabetic patients to present with cortical cataracts and a myopic shift, particularly if their blood sugar is uncontrolled.
Posterior Subcapsular Cataract
- Characterized by opacification at the posterior side of the lens, closest to the vitreous.
- More common in younger patients than nuclear sclerotic and cortical cataracts.
- Often smaller than nuclear sclerotic and cortical cataracts, but often associated with a profound increase in glare.
- Has a profound effect on near vision (this is because as you focus on near objects, along with your lens changing shape, your pupil also constricts – this causes the cataract to affect more of your visual field during near viewing!).
- Can be associated with corticosteroid use.
Traumatic Cataract
- Characterized by a unique star-shaped opacification.
- Can be caused by blunt trauma or different forms of ocular injury.
- Usually have a profound effect on vision and is often associated with injury to other parts of the eye, such as the iris.
- More likely to be unilateral than the other types of cataracts (but remember to rule out other ocular disease, such as retinal detachment, angle recession, etc!)
Congenital Cataract
- Just as the name implies, this type of cataract is present at birth, so think of this when examining a cataract in a pediatric patient!
- Approximately 50% are genetic, so make sure to ask about family history.
- May also be due to secondary causes such as uveitis, diabetes, etc.
- Often leaves patient with asymptomatic vision, but not always (if vision is affected, lens removal and IOL implantation is indicated).
- May have many different presentations, such as cerulean cataracts, anterior polar cataracts, or many others.
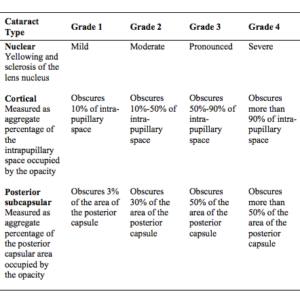
Tips for Grading Cataracts
Sometimes, during a clinical exam, it can be tough to tell what type of cataract you’re looking at, especially if your patient has 1mm undilated pupils. Here are a couple clinical tips to help nail down exactly what you’re seeing:
- RETROILLUMINATION: seriously, retroillumination can be your best friend when grading cataracts. It’s particularly useful for cortical cataracts by clearly demarcating cortical spokes or vacuoles (especially those located peripherally on the lens!). It is also a very useful technique in identifying posterior subcapsular cataracts because it makes an opacity that is located in a thin layer of the lens prominently visible.
- Look for associated lenticular signs: for example, cortical cataracts are often associated with vacuoles, and nuclear sclerotic cataracts are associated with brunescence.
- Use your brain! Take into consideration other aspects of the exam besides slit lamp – if the patient can’t see out, you can’t see in! Were you able to get good views of the retina during BIO? What was the patient’s best-corrected visual acuity? You should keep all this information in the back of your mind when looking at cataracts.
- Use well-respected clinical guidelines, such as the AOA’s Care of the Adult Patient with Cataracts or
- Remember, it’s not uncommon for there to be multiple kinds of cataracts (i.e. compound cataracts) in patients! For example, if you observe cortical spoking and nuclear opacification, your patient likely has both cortical and nuclear sclerotic cataracts!
Be sure to catch Part 2 of our Cataracts Awareness series about how to manage cataracts and the different forms of treatment!

